Limb Preservation
Dr. Kolodenker specializes in Diabetic Foot and Ankle Wound Care. Foot or Ankle ulcerations and Limb Salvage, preservation.
Please contact Dr. Kolodenker for an appointment 949-651-1203
A foot ulceration forms when there is increased pressure on a body part like the foot, ankle or toes.
Once the pressure is relieved, the body will naturally close the wound.
There are ways to speed up ulceration healing.
Increasing blood flow, local wound care, grafting, correct shoes, surgical intervention are all ways to speed up ulceration closure.
Amnio grafts and stem cell treatement is something we do here in the office
Wounds & Ulcers
A foot wound is a cut, abrasion, or other type of damage to the skin and tissue of the foot. When diabetic foot wounds do not heal or keep returning they can become ulcers.
Diabetic foot ulcers are chronic wounds or sores which can deepen and extend through all layers of skin, and impact tendons, bones, and other structures within the body. These ulcers are also the principal portal of entry for infection in patients with diabetes and, left untreated, can spread and present far more severe complications.
Causes of Diabetic Foot Wounds
Some factors that contribute to the formation of wounds on the feet include wearing tightly fitted shoes, getting a pebble stuck in your shoe, stepping on something sharp, or wearing shoes that rub against your skin or apply repeated pressure.
It is important for people with diabetes to check their feet daily because they may not be able to feel when a small cut, abrasion, or repeated pressure causes a wound in the skin. This is because they may also be experiencing neuropathy, which is a type of nerve damage and a complication of diabetes that can cause a loss of feeling in the feet. If a diabetic person no longer has feeling in their feet and a wound develops, it’s very possible a wound may go unnoticed if they are not inspecting their feet daily.
What may appear to be just a small inconvenience such as a blister, callus, or small wound can worsen over time, so it’s important to be safe and seek the prompt attention of Dr. Kolodenker who is a specialist in diabetic wounds, ulcers, and diabetic infections in feet, ankless and toes. If you’ve developed a wound, Dr. Kolodenker suggests staying off of the foot until you are able to meet with him for a full examination and analysis of your wound.
Why do Diabetic Foot Ulcers form? How to treat Neuropathy
In order to develop a foot ulcer some form of Neuropathy must exist.
About 50% of patients with newly onset diabetes do not know they have Neuropathy.
Ask your doctor to check. The test takes 5 seconds to do and most physicians that treat diabetics can do it. The tool is a Semmes-Weinstein Monofilament.
Diabetic Foot or Ankle ulcers will develop in an area of pressure 99% of the time.
Get rid of the pressure and you will cure the ulcer. Simple!!!
Your body naturally builds up a callous in an area of pressure. Think about what happens to your hands after gardening or sweeping. Your body has a natural way to protect itself. Diabetes messes up the protective mechanism.
As your Hemoglobin A1c (HbA1c) goes up, so does your chance of amputation. Watch your glucose levels! Please.
As the callous grows, the pressure under it continues to increase. Since Neuropathy impedes the ability to feel pain, the increased pressure rubs away a hole in the skin( an ulcer).
Prevent ulceration by preventing Neuropathy.
Prevent Neuropathy by making sure your glucose and HbA1c are within normal limits.
If you already have Neuropathy, diabetic shoes and diabetic specific vitamins help decrease chance of ulceration.
Non-Diabetic Foot Ulcers
Not everyone with an ulceration has diabetes. Foot ulcers may form in individuals who are suffering from poor circulation (due to conditions such as arteriosclerosis or venous insufficiency), kidney damage, hypertension, lymphedema, nerve damage (neuropathy) inflammatory diseases or other medical conditions.
Any abnormality in the muscles or bones of the feet may also lead to a foot ulcer, particularly when shoes do not properly accommodate the altered shape of the foot.
Dr. Kolodenker recommends that individuals with any of these conditions also examine their feet daily. If any breaks or redness caused by pressure points are spotted, he advises staying off the feet and making an appointment as soon as possible.
Treating a Foot Wound or Ulcer
Ulcers are usually covered by callus or fibrotic tissue. These ulcers are typically painless. This makes the trimming of hyperkeratotic tissue (thickened skin or callus) important for comprehensive wound evaluation.
Adequate debridement is the first step in the evaluation of a foot ulcer. In the debridement process, Dr. Kolodenker cleans, disinfects, and removes dead (necrotic) or nonviable tissue, bacteria, hyperkeratotic tissue, and foreign debris from the wound. This creates an environment on the foot that is conducive to healing.
After debridement, Dr. Kolodenker will probe the wound with a sterile blunt instrument to determine the involvement of underlying structures, such as tendons, joint capsules or bones.
An X-ray will follow, where Dr. Kolodenker will look for soft tissue gas and foreign bodies, and evaluate the ulcer for bone involvement. The involvement of underlying structures and the presence or absence of ischemia and/or infection must be determined before Dr. Kolodenker can appropriately classify the wound and implement the necessary treatment plan.
You will likely be advised to rest the foot and keep pressure off of the wound while it heals. Dr. Kolodenker may also prescribe custom orthotics, pads, and other devices which will offload pressure on the wound.
As an expert Foot and Ankle Wound Care Specialist that deals with Ulcers, Wounds, and Diabetic Infections, Dr. Kolodenker is devoted to closing non-healing open foot wounds in his patients and helping them prevent the worse case scenario. His wound care treatments often heal within a few weeks. He has devoted his practice to wound care and amputation prevention, and also repairs Charcot Deformities which allow foot wounds to heal.
Diabetic Wound and Ulcer Prevention
Recognition of risk factors, preventive foot maintenance and regular foot examinations are essential in preventing foot ulcers in patients with diabetes.
Dr. Kolodenker maintains that meticulous attention to foot care and proper management of minor foot injuries are key to preventing wounds from developing. Daily foot inspection by the patient or caretaker should be performed to check for any cuts, scrapes, sores, wounds or discoloration. If any changes are detected, an appointment with Dr. Kolodenker should be made as soon as possible.
The feet should be gently cleansed with soap and water, followed by the application of topical moisturizers. Avoid hot soaks, heating pads and harsh topical agents.
Toenails should be trimmed straight across and not too short. Dr. Kolodenker also suggests wearing shoes both inside and outside the home to protect the feet from injuries.
Shoes must fit comfortably and there is ample room for your toes. Custom shoes and insoles to offload pressure and pad the feet can be very beneficial. Medicare covers the cost of custom shoes and insoles for patients that qualify. Another great way to prevent venous ulcers is via compression therapy (compression stockings).
To ensure patients are doing all they can to prevent a diabetic foot ulcer (DFU) from developing, these individuals are encouraged to schedule an appointment for a diabetic foot screening and to receive professional guidance. If arterial disease is present then a consultation with a Vascular Surgeon is very important.
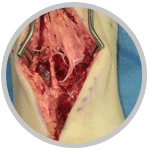
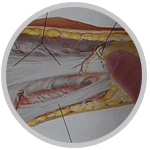
Split Thickness Skin Graft in Wound Care
Skin grafts are used to cover and heal wounds and ulcers. The graft can be harvested from various sites on the patient’s own body. Dr. Kolodenker most commonly uses the calf or the thigh for the surgical donor site. Grafts that are taken from the patient have the best chance of incorporating, and the chance of rejection is low.
There are also synthetic grafts that can be placed on a wound. These grafts are safe and spare the patient from a harvest site procedure. Dr. Kolodenker can usually tell within 3-5 days after skin graft surgery if the graft has taken.
After placing the skin graft, Dr. Kolodenker will apply a wound vac for 3-5 days. This is a therapeutic technique using suction, tubing and dressings to remove excess fluid and promote healing in the wound site.
Skin grafts are also helpful in preventing more proximal amputations, which are those that are closer to the center of the body.
Stem cell grafts have become a great modality.
Amputation Prevention
Dr. Kolodenker has devoted his career to closing non-healing wounds in his patients, and helping to prevent amputations. He has helped save toes, feet and legs in patients with diabetes, peripheral vascular disease, vasculitis, and more. He uses the most modern technology and everything possible to prevent amputations—particularly more proximal foot or leg amputations, which are those that are closer to the center of the body.
Preventing a below-the-knee amputation is crucial to good health. By keeping a foot, patients will not need to wear prosthesis and can get out of bed and move in case of an emergency. Studies have shown that having a below-the-knee amputation increases stress on the heart and decreases life expectancy in people with diabetes and vascular disease.
By keeping their toes, feet or legs intact, patients will live longer. Surgical intervention for diabetic ulcers and wounds can speed up the recovery time to help avoid amputations from being necessary. Dr. Kolodenker’s wound care treatments often heal within a few weeks and patients can often avoid amputation. Before you have surgery anywhere else, make an appointment with Dr. Kolodenker so he can perform a diabetic foot screening and provide you with his expert opinion.
When Amputation is Unavoidable
People with diabetes are more at risk of having a leg or foot amputated due to complications from ulcers and ulcer infections.
With prevention and early professional care, many amputations can be avoided. Sometimes, however, when the patient has uncontrolled diabetes or poor arterial blood flow, this type of surgery is necessary to stop the infection in the foot from spreading to other parts of the body.
Transmetatarsal Amputation (TMA)
A Transmetatarsal amputation (TMA) is a surgery which treats a severely infected foot and is performed to prevent the infection from spreading, while saving the limb. The procedure involves removing part of the foot: resectioning all tissues across the metatarsals in the forefoot. The level at which the resection is performed depends on the degree of tissue necrosis. It is ideal to leave as much tissue as possible.
Wound Care
Cleaning the wound
Saline wash is used before application of any wound care product. Dr. Kolodenker advises saline wash is the way to clean the wound. Be sure to dry well after use, using sterile gauze to dry the wound.
Bandages
Keeping the wound clean and dry will need a lot of gauze. Dr. Kolodenker suggests ordering bandages online to save time and money. You should also save the receipt and submit to insurance for reimbursement, which may require a prescription from the doctor.
How to Care for Very Wet Wounds
Betadine is used for very wet wounds. It is great between the toes or macerated skin (skin that has become softened from soaking in liquid). Topical Iodine and Betadine are the same thing. Consult with Dr. Kolodenker before using as prolonged use is not ideal for wound healing.
Wound Care Products
MediHoney
MediHoney is a great agent to speed up healing. It works just as well, if not better, than Santyl and is much more affordable. Dr. Kolodenker usually advises patients to apply it to the wound once a day. MediHoney is sometimes used instead of a topical antibiotic ointment.
Silver Alginate
Silver Alginate is also a good product to absorb moisture and create a mesh grid environment for healing. Silver is a natural antimicrobial. This would be changed every 1-3 days. It can be combined with MediHoney for a faster healing result.
For a full list of our wound care products, please visit our products page.
Last Update 06-26-2022
Achilles Rupture
Ankle Arthroscopy

Ankle Fracture

Ankle Sprain
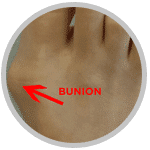
Bunion

Custom Orthotics

Foot Pain
Heel Pain
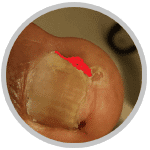
Ingrown Toe Nail

Laser Nail Fungus

Plantar Fasciitis
Full Symptoms List
Ankle Replacement Surgery
Arthritis
Achilles Tendonitis
Achilles Tendonosis
Achilles Tendon Rupture
Adult Flatfoot
Ankle Fractures
Ankle Sprain
Arthroscopy
Bunions
Callus
Cavus Foot
Calcaneal Apophysitis
Calcaneus Fracture
Cartiva
Charcot Foot
Chronic Lateral Ankle Pain
Chronic Lateral Ankle Stability
Clubfoot
Coalition
Corn
Diabetic Foot
Fifth Metatarsal Fracture
Foot Fracture
Foot Pain
Fungus
Ganglion Cyst
Gout
Haglund’s Deformity
Hallux Limitus Rigidus
Hammer Toe
Heel Fracture
Heel Pain
Ingrown Nail
Intoeing
Laser Toe Nail Fungus
Lisfranc’s Injury
Metatarsalgia
Neuroma
Neuropathy
Open Fracture
Orthotics
Osteochondral Defects
Pediatric Flatfoot
Peripheral Vascular Disease
Peroneal Tendonitis
Plantar Fasciitis
Plantar Wart
Platelet Rich Plasma, PRP
Polydactyly
Posterior Tibial Tendon Dysfunction
Rheumatoid Arthritis
Scars
Sesamoiditis
Sever’s Disease
Smelly (Malodorous) Feet
Stress Fractures
Tailor’s Bunion
Talus Fracture
Toe Fracture
Topaz
Turf Toe
Warts
↑ TOP
Ankle Replacement Surgery
A great option for arthritis in the ankle. Usually patients with arthritis are thinking about an ankle fusion or a replacement.
Arthritis
Arthritis of a joint is when the normal cartilage has broken down and bone is rubbing on bone. This creates pain and inflammation.
Achilles Tendonitis
Acute inflammation of the achilles tendon. Pain is usually on the back of the heel or ankle.
Achilles Tendonosis
Chronic injury to the achilles tendon. This results in thickening of the tendon around the insertion.
Achilles Tendon Rupture
Basketball and soccer injuries are the most common reason to rupture the achilles. Can happen during any running or jumping activity.
Adult Flatfoot
By itself, there is no need to treat. Painful flatfoot should be treated.
Ankle Fractures
The bones inside of the ankle joint are broken. Depending on the fracture type, surgery might be needed.
Ankle Sprain
The most common sports injury. Sprains can be mild or severe.
Arthroscopy
Placement of a camera inside of a joint with small incisions. Usually in the ankle.
Bunions
Bump on the big toe joint. Mostly a genetic deformity.
Callus
Thickening of skin due to pressure or irritation.
Cartiva
Implant used to treat arthritis in the big toe joint.
Cavus Foot
A foot with a higher arch. Treatment needed if there is pain.
Calcaneal Apophysitis
Irritation of the growth plate at the back of the heel bone. Seen usually in kids that do lots of running.
Calcaneus Fracture
Break in the heel bone. Usually due to a fall.
Charcot Foot
Usually seen in patients with diabetes. The joints and ligaments give out and the foot collapses.
Chronic Lateral Ankle Pain
This can be due to a tendon injury or ligament injury.
Chronic Lateral Ankle Stability
Chronic ankle sprains will cause this. When physical therapy fails, surgery is a good option.
Clubfoot
A deformity seen at birth. Early stretching and casting is key.
Coalition
An abnormal growing of bones that should typically be separated.
Corn
Much like a callous. Forms from high pressure.
Diabetic Foot
Needs extra attention due to higher risk of infection. A Podiatrist is the best option to treat any diabetic foot problems.
Fifth Metatarsal Fracture
A common injury after ankle sprains. Displacement will determine the need for surgery.
Foot Fracture
There are many bones in the foot and any of them can break. A Podiatrist is best for any foot injury.
Foot Pain
So many causes of foot pain. Going to see a good Podiatrist will get you back on your feet faster.
Fungus
Foot fungus can lead to athlete’s foot infection.
Ganglion Cyst
A benign growth. Usually seen around joints or tendons.
Gout
When uric acid leaks out of joints and creates intense pain.
Haglund’s Deformity
Extra growth of bone on the back of the calcaneus.
Hallux Limitus Rigidus
Arthritis of the big toe joint. Can be genetic or seen decades after an injury. Most patients do not remember the injury.
Hammer Toe
Contracture of tendons of the toes. This causes toe deformities.
Heel Fracture
One of the worst injuries of the foot. Usually due to a fall.
Heel Pain
Plantar fasciitis is the most common reason for heel pain. Good shoes and stretching will be needed to cure.
Ingrown Nail
When the corners of the nails or back of nail digs in the skin. This can cause an infection. Removing the ingrown is the best treatment option.
Intoeing
Internal hip rotation is the most common reason for intoeing. Monitoring and/or PT is advised.
Laser Toe Nail Fungus
Use of a laser to get rid of fungal nails. Safe and effective.
Lisfranc’s Injury
A frequently missed injury. An MRI is needed to rule out.
Metatarsalgia
Pain on the metatarsals. Due to increased pressure on the ball of the foot.
Neuroma
Nerve enlargement. Usually due to shoes that are too narrow.
Neuropathy
Loss of normal sensation in the nerves.
Open Fracture
A fracture and an open wound together. The open wound connects to the fracture.
Orthotics
Custom orthotics are used to help with alignment and decrease pain.
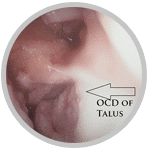
Osteochondral Defects
Cartilage injury. Usually seen in the talus bone.
Pediatric Flatfoot
Monitoring is typically advised. Rarely is treatment suggested.
Peripheral Vascular Disease
Poor blood flow. Usually arterial in nature. Can sometime be venous.
Peroneal Tendonitis
The lateral ankle tendons become irritated.
Plantar Fasciitis
The most common foot injury. Good shoes and stretches is key. Early treatment is very important. We have lots of information to cure plantar fasciitis on this website.
Plantar Wart
A viral infection of the skin. Very common around swimming pools.
Platelet Rich Plasma, PRP
Spun down, concentrated healing cells. These are injected in areas of arthritis, tendinitis, inflammation.
Polydactyly
Multiple digits. Usually fixed when the patient is at least 6 years old.
Posterior Tibial Tendon Dysfunction
Very similar to shin splints. Pain a the tendon from an over pronated foot.
Rheumatoid Arthritis
An autoimmune disease that will result in pain and deformity. Not all patients with RA will develop deformities.
Scars
When tissue does not heal up as well as possible. Silicone is good to decrease scars. Cortisone injections are sometimes needed.
Sesamoiditis
A very stubborn injury. Offloading is key. Custom orthotics, walking boot, cast.
Sever’s Disease
Calcaneal apophysitis. Irritation of the growth plate on the back of the heel.
Smelly (Malodorous) Feet
Usually seen in patients that sweat a lot.
Stress Fractures
Occur from overuse and bad shoes.
Tailor’s Bunion
A bunion on the outside of the foot. Also knows as a bunionette.
Talus Fracture
Fracture of the talus bone. Usually due to high impact. High risk of AVN.
Toe Fracture
Very common injury. The little toe is constantly injured on furniture. Compression bandage or buddy tape is advised.
Topaz
Ablation treatment for stubborn tendon injuries.
Turf Toe
Hyperextension of the big toe joint. Common in football. Strain of the ligaments.
Warts
Viral infection in the skin. Very common in areas where people are bare foot together.
Last Updated 05-05-2022